Treating Fibromyalgia
Massage Therapy as a Beneficial Tool
Originally published in Massage & Bodywork magazine, February/March 2004. Copyright 2003. Associated Bodywork and Massage Professionals. All rights reserved.
Most massage therapists and bodyworkers have seen the effects of fibromyalgia on at least some of their clients’ bodies and minds. Often unable to find help elsewhere, fibromyalgia sufferers have been known to seek out alternative methods to find lasting pain relief. Understanding the disorder more comprehensively and discovering how massage can be applied to a particular client may benefit all who suffer from it.
A Fibromyalgia Primer
Fibromyalgia (FM) is a chronic musculoskeletal condition expressed in widespread pain over the entire body. FM patients (a higher percentage of whom are women than men) also suffer from tension headaches, fatigue, stiffness and sleep disorders. It is estimated that 7 million Americans are afflicted with fibromyalgia — their pain and fatigue in some cases being so severe that the individual spends entire days in bed.
As recently as 18 years ago, the U.S. medical community recognized FM largely as a psychosomatic disorder, not a physical condition. Physicians would conduct lab tests and X-rays to find evidence of rheumatoid arthritis, osteoarthritis and other pathologies that produce pain in muscles and tendons. Of course, with FM the ultimate culprit, these tests showed nothing. In most cases, the patient appeared to be physically normal, hence the psychosomatic diagnosis.
Today, FM is diagnosed in most cases of fatigue, insomnia and other sleep disorders, regardless if “algia” (pain) is present or not. Even though the last 18 years of scientific research has added a wealth of information to the discussion of FM diagnosis, it has not clarified an already existing confusion — what causes FM onset?
There is an evolving theory that attempts to explain a chain of pathological events responsible for the development of FM. This theory (the supporters of which believe it is not an abnormality of the muscular system) states that the concentrations and activities of neurotransmitters are changed as a result of an unknown trigger such as trauma, sleep disorders, hormonal changes, stress, chemical exposure, etc. These changes mark the first step in the development of FM. Numerous studies have confirmed that FM patients show a decrease in their serotonin concentrations. From this point of view, only one reasonable approach is recommended : serotonin reuptake inhibiting medications (Prozac, Paxil, etc.), sedative medications, muscular relaxants and exercises to increase natural endorphin production. Years of such treatment, however, have failed many individuals. FM has now reached pandemic proportions and patients caught in this web sooner or later may find their lives ruined.
We believe that FM is actually a fibromyositic pathology. Fibromyositis is a chronic, low-grade inflammatory condition of the muscle, fascia and other connective tissue. The main cause of fibromyositis is the accumulation of pathological hypertonus in muscles over a prolonged period of time. This can be triggered by post-traumatic phenomena, stress, sleep disorders, hormonal changes (thereby explaining the high incidence of women), toxic chemical exposure and other factors.
Finding a New Theory
In order to better understand how massage can help in cases of FM, a short discussion of anatomy and pathology is appropriate. As we all know, muscles are surrounded by fascia. This connective tissue plays an important role in the determination of the extent of muscle stretch and contraction. It is very important to understand that fascia also provides pathways for nerves and blood vessels. In cases of FM, due to the prolonged pathological hypertonus in muscles, fascia becomes tense causing compression of muscle fibers, nerve tissue and blood vessels. This kind of irritation first initiates, and later brings about the development of, fibromyositis. The condition of constant muscle tension in FM cases creates an overload (strain) on muscles and tendons. Strain always leads to the development of inflammation .
The persistence of this inflammatory condition prompts calcium deposits in muscles and tendon attachments to the periosteum — in other words, fibromyositis. A chronic inflammatory condition of the skeleto-muscular system causes secondary changes in neurotransmitter levels and activities in the central nervous system. The changes appear after the patient starts to experience chronic pain . In such a case, the initial trigger is in the skeletal muscles where local, pathological abnormalities were developed.
Authors of many studies have detected significant depletions of adenosine tri-phosphate (ATP) concentration, as well as other high-energy phosphates in the skeletal muscles of FM patients (Bengtsson et al., 1986; Larsson et al., 1988; Bennett, 1991; Park et al., 1998). ATP is a major energy source for muscular contraction. When a nervous command arrives through a motor neuron to a skeletal muscle to produce a contraction, ATP molecules are used. This energy causes the actin and myosin to attach to, and slide past, one another during muscular contractions. When a muscle needs to relax, it again uses ATP molecules to detach myosin from actin. It is important to remember that constant (chronic) muscular hypertonus uses and exhausts the stores of ATP.
Imagine a situation where the concentration of ATP is decreased. The motor commands arrive from the central nervous system to the muscles, and muscular contraction is achieved using available ATP. However, when the muscle needs to relax, ATP is in short supply, as most of it has been used in the contraction. In such a case, some of the muscle fibers remain in the contracted state, even during periods of relaxation. New nervous commands arrive, and again, all available ATP is used to produce a contraction. This is how tension starts to build. The more tension builds up in skeletal muscles, the more tension we can find in the fascia, aponeurosis and other soft tissues. Tension causes a decrease in elasticity, and it starts to affect microcirculation. A mismatch between motor nervous commands and insufficient arterial blood supply initiates changes in the local pH, followed by the activation of pain receptors. It’s at this time the patient starts to feel pain.
After several weeks or months (depending on the individual) of such bombardment of the central nervous system with chronic pain, changes in neurotransmitter activities and concentrations become apparent. The level of substance P (a neurotransmitter responsible for the slow or chronic pain conduction through the spinal cord) increases and the level of serotonin decreases. Serotonin is a very important neurotransmitter, mediating basic bodily functions such as smooth muscle contraction (especially digestive system musculature) and blood coagulation. Additionally, serotonin acts as a neurotransmitter in the brain. It is responsible for our wakeful state and excitement. Patients with clinical depression, which frequently accompanies FM, show a significant decrease in the concentration of serotonin in the brain. All examined FM patients exhibit an increase in the concentration of substance P in the spinal cord, which in most cases is the result of a decreased pH level in muscles.
Important findings supporting this theory are pathological changes found in the muscle cell mitochondria (Bennett, 1991), as well as a decrease in magnesium concentration (Abrahams and Flechas, 1992). Mitochondria are the power plants of the cell, synthesizing ATP (magnesium is a mediator in ATP synthesis). Numerous mitochondria are found within each cell. When ATP is depleted in the skeletal muscles of FM patients, an “energy crisis” (Eisenger, 1992) is created, triggering the entire clinical picture.
Comparing Fibromyalgia and Myofascial Pain
As you see, this concept has a completely opposing approach to the pathogenesis and the treatment of FM that is currently practiced. The key is in the skeletal muscles that have developed pathological abnormalities. The abundant clinical picture of FM is a secondary reaction, triggered by chronic pain followed by changes in the neurotransmitters. From this point of view, the initial target of the treatment is skeletal muscles, fascia and other connective tissue. Very frequently, myofascial pain syndrome (MPS) is misdiagnosed as FM. Therefore, it is important for the massage practitioner to understand the difference between these abnormalities.
The clinical picture of MPS is usually much more acute. In the areas of the trigger points, the pain is more intense with a radiating pattern along the same muscle or muscle group. The patient complains of a decrease in the range of motion, as well as a significant weakness in muscles containing active trigger points. The patient feels better when the muscle is at rest, and the intensity of the pain increases as soon as the affected muscle starts to contract. One of the main clinical differences between FM and MPS is the distribution of pain. In MPS, the pain has local character and if it radiates, the patient feels it along the same segment. MPS affects all age groups and both genders. There are no accompanying syndromes. Please note that sharper levels of pain do not bring about a decrease in serotonin level. Rather, a low-grade persistent pain such as in FM, is the causative factor in serotonin level decrease.
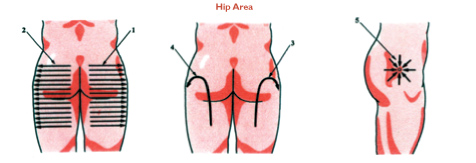
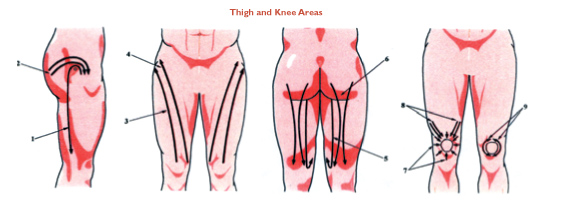
The clinical picture of FM is much more complicated. The intensity of the pain in FM is much lower, but it is persistent. Pain is present regardless of contraction or relaxation of affected muscles. Low-grade, persistent, psychologically-exhausting pain is one of the main symptoms of FM. Another difference is poor localization of pain, which seems to affect other soft tissues as well (e.g., skin, fascia and periosteum). Finally, the FM patient may exhibit pain either over the entire body or have patchy localizations of pain. In the case of the latter, affected areas are separated by unaffected areas. For example, the patient will complain of headaches, pain in the lower back and gluteal areas, and in the plantar fascia of the feet.
Contrary to MPS, FM carries a very strong psychological component. The patient is usually depressed, suffers from mood swings, easily bursts into tears, has significant sleep disturbances, and is mentally and physically fatigued. Additionally, the patient may have many related physical complaints: migraines, bruxism (teeth grinding), TMJ problems, irritable bowel syndrome, pelvic pain, tachycardia (increased cardiac rate), Raynauld’s phenomenon and chronic rhinitis.
The pain-causing physical expressions of chronic inflammation consist of mild swelling of the soft tissue, tension in fascia, pathological hypertonus of muscles, significant decrease in blood supply and calcium depositing in the soft tissue.
FM Treatment
Because poly-fibromyositis is a chronic condition, one must remember that the first three to four treatments can possibly aggravate the clinical picture. For an unclear reason, only 10 percent of FM clients react with aggravation of pain. In any case, we recommend that the FM client be informed of the possibility of reaction. The reason for this aggravation of pain is the intense stimulation of oxygen supply to the “hungry” cells and the excessive release of toxic waste products from the tissues into the circulatory system. Usually, however, during the first 10 to 15 correct massage therapy treatments, the client can, in fact, notice clear, significant positive changes. One must keep in mind, however, that the healing process requires time.
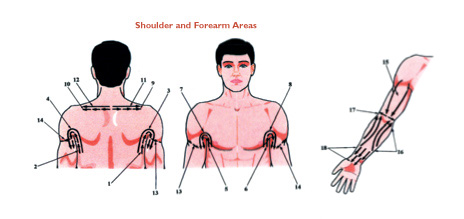
We recommend beginning the first 10 massage therapy treatments on a two procedures per week basis. Remember that FM clients complain of sharper levels of pain in certain regions (such as neck and upper back, or lower back, including the buttocks regions, etc.). We believe that in such cases, massage therapists must focus on those regions. However, the full-body massage treatment should be considered after the first three to four treatments. Also keep in mind that lying on the stomach for more than 12 minutes at a time is not recommended for the FM client, because the pressure on the rib cage transmitting to the rib attachments can cause additional tension in the muscles. Therefore, consider treating the neck and upper back region in a side-lying position, with a towel placed between the neck and pillow. When the client is prone, we recommend placing one pillow under the stomach and two pillows under the chest. Do not treat FM clients using a massage chair.
We also maintain that exercise is very beneficial for FM clients. It is important to keep in mind, however, that the exercise program should not begin prior to the first 10 sessions of massage therapy. Many clients have severe reactions to exercise if not prepared for active movements by a series of massage procedures.
After the first 10 treatments, the client has to begin a combination of exercise (at least two to three times a week), with special massage therapy for FM (five additional treatments). After a two-week break from massage therapy (keep in mind that the exercise program does not get a break), it is important to come back for a series of 15 massage therapy procedures (at least twice a week) and continue the exercise program (at least four times a week at this point). Usually, after the first 30 massage therapy procedures and continued exercise, FM symptoms (such as pain all over the body, sleeplessness, tension headaches, chronic fatigue) become much less severe. Even though the client may think that she feels better, she must still continue to receive treatments and maintain her exercise program. After a three-week break from massage therapy, the client must return to at least one massage therapy procedure every week and, of course, still continue to exercise at least four times a week. This is the only way to prevent re-accumulation of tension in muscles.
Some experts have recommended that FM clients employ various types of aerobic and stretching exercises for their condition. From our knowledge and experience, we can say that the most beneficial exercise program for FM clients revolves around rehabilitative exercise routines (making sure that the neck, shoulders, upper back, lower back, hips and knees are exercised separately). Clients should be advised not to force any movements when they exercise. If, for example, a left head rotation produces even the slightest pain, the movement must stop, and the head must be turned toward the center. It is also important to advise the client to perform the exercises slowly, as any aggressive exercise may aggravate the symptoms significantly.
History’s Lessons
In 1968, in Dnepropetrovsk, Ukraine, in the former Soviet Union, workers of a large industrial complex started developing fibromyalgia symptoms in epidemic proportions. The Soviet government assigned a group of scientists to find the causes of this epidemic. It was clear to everyone that psychosomatic disorders should be ruled out.
The group of scientists eventually found that an adjacent lake, heavily contaminated with toxic waste, was causing muscular tension. Over time, this led to the development of fibromyalgia. What these scientists learned was that individuals suffering from myofascial pain syndrome have a higher risk of developing fibromyalgia. But those who develop fibromyalgia are almost guaranteed to develop chronic fatigue syndrome.
During a study and clinical treatments, these scientists concluded that the development of fibromyalgia and chronic fatigue syndrome can be prevented by medical massage treatments (for more on medical massage, see Boris Prilutsky’s medical massage article in Massage & Bodywork, August/September 2003). As we mentioned here, the persistence of low-grade pain bombards the central nervous system and causes a decrease in serotonin level. Restoration of ATP, neuromuscular function and stabilization of metabolism will decrease the pain sensation. The elimination of low-grade pain will allow the central nervous system to restore the level of serotonin and chronic fatigue syndrome development will be prevented.
The Way Forward
In our decades of practical experience, we have treated many cases of classic fibromyalgia. We can report that in most cases, symptoms such as fatigue, general body pains, headaches, stiffness and sleeplessness were significantly reduced following a series of massage therapy sessions. We strongly believe that a correctly formulated medical massage protocol is the main tool in effective control and elimination of FM symptoms. Proper nutritional support, exercise, psychological assistance and other types of therapy are equally important components. But they should be employed later when the pain sensation and stiffness are significantly reduced.
It was almost three decades ago in the former Soviet Union that scientists researched and established the theory of fibromyositis development as a main cause of FM. They also developed a method of massage therapy treatment that we’ve described here. The main goal of this article is to share with practitioners the optimal protocol of medical massage in treating fibromyalgia cases and to enable massage therapists to share this concept with other healthcare practitioners.
Medical Massage Techniques
(with lubrication)

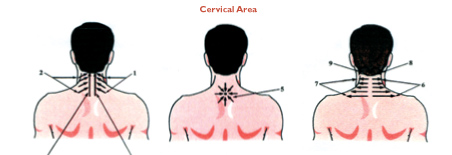
Figure 1: Client lies on her side. Place a folded towel between the neck and pillow. Place fingers around the occipital bone at the insertion of neck muscles to the skull. Gradually massage the region, while increasing pressure, for three minutes.

Figure 2: Stand in front of client; place both hands on the neck. Perform petrissage No. 1 on the lateral part of the neck and upper trapezius. This petrissage is a kneading technique where the thumbs act as barriers for soft tissue movement, and the four fingers mobilize soft tissue in the direction of the thumbs. Both hands perform the same action simultaneously. Do not massage the carotid artery.

Figure 3: If possible, place the arm of the client behind her back. Place a hand on the anterior part of the shoulder joint for support. With the top of the fingers of the other hand, massage under the scapula area. If it is difficult or impossible for the client to place her arm behind the back, perform the sub-scapular mobilization in a normal position.

Figure 4: Perform petrissage No. 2 on the lateral part of the neck and upper trapezius. Petrissage No. 2 is a kneading technique where the thumbs act as barriers for soft tissue movement and four fingers mobilize soft tissue in the direction of the thumbs. This technique is not simultaneous — each hand follows the other.

Figure 5: Place both thumbs on the lateral part of the neck as close as possible to the occipital bone. Thumb after thumb, massage the entire lateral side of the neck.

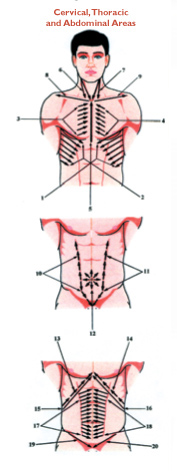
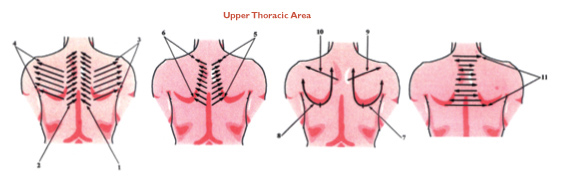
Figure 6: The client lies on her stomach. Place your right palm on the lower back region. Place your left hand on top of the right hand. With application of initial pressure, perform ironing techniques from the bottom up on all areas of the back. Upon reaching the upper part of the back, disconnect the hands and return to the lower part without contact.

Figure 7: Place the back of the fingers on the lower part of the back and, with initial pressure from the bottom up, massage the entire area of the back. Upon reaching the upper part of the back, disconnect the hands and return to the lower part without contact.

Figure 8: Place the hands on the lateral parts of the back. Under initial pressure, massage the entire back, hand against hand in a manner of cross-fiber friction.

Figure 9: Perform petrissage No. 1 and No. 2 on the entire area of the back.

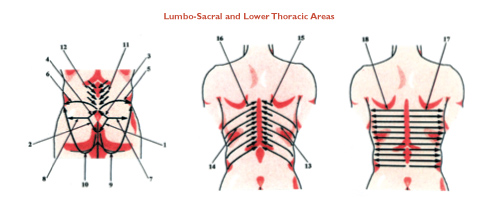
Figure 10:Connective tissue massage can release tension in myofascial tissue.
